How is MS diagnosed?
Get an overview of the tests neurologists may use when diagnosing MS such as an MRI scan, lumbar puncture and neurological examination. Like MS, every diagnosis story is different.
A lumbar puncture is one of the tests that can be used to help diagnose MS. It involves removing and analysing a sample of cerebrospinal fluid (CSF), the fluid that surrounds the brain and spinal cord within the skull and backbone. It is sometimes referred to as a spinal tap.
On this page we look at what is involved in having a lumbar puncture and how it can help with the diagnosis of MS.
Your medical history and initial tests such as a neurological examination and an MRI scan may not give enough evidence to make a diagnosis of MS. If this is the case, then a lumbar puncture can help confirm a diagnosis of MS or help rule out other conditions.
Having a lumbar puncture can be uncomfortable or unsettling, but it is a common, low-risk procedure.
A lumbar puncture appointment will be about an hour, but the procedure itself typically takes about 20 minutes to half an hour. It will be performed by a doctor or specialist nurse.
You will be asked to lie on a hospital bed/couch on your left-hand side and to draw your knees up to your chest in a foetal position. The doctor will then feel around your lower back to identify the right position to insert the lumbar puncture needle in the area of your spine below the spinal cord but above your pelvis.
If they are struggling to find the right area, you may need to have the procedure sitting upright, similar to an epidural commonly used during childbirth. It is easier to find the right spot in this position, but the side position is preferred as it allows for a reading to be taken to assess the pressure of the cerebrospinal fluid (CSF) before samples are taken.
Once identified, the area will be marked and then cleaned to reduce the risk of infection. You may have drapes put over the area. A local anaesthetic will be injected to numb the skin, so you don’t feel the lumbar puncture needle as it is inserted. The local anaesthetic usually only takes a few minutes to take effect.
The lumbar puncture needle is longer and thinner than a needle that would be used to take a blood sample. This is so it only leaves a small hole when removed. The needle will be partially inserted, then if you’re lying on your side, before samples are taken, a manometer will be used to take a pressure reading. Finally, a quantity of cerebrospinal fluid will be drawn off. The CSF comes out of the thin needle in small drops. Usually around 20 drops will be collected in each of three tubes. The needle is then removed.
The fluid is then sent for analysis to look for markers of inflammation.
Watch consultant neurologist Nick Cunniffe explain how to prepare for a lumbar puncture and what is involved.
There is always a very small risk of infection when a needle is introduced into the body. The doctor will wash their hands, wear sterile gloves, and clean the area thoroughly to reduce the risk of infection.
There is a small risk of bleeding once the needle is taken out, so you will usually be asked if you’re taking any blood thinners as they can prevent a clot from forming if you do bleed.
By far the most common side effect is a headache, with around 3 in 10 people experiencing a headache following a lumbar puncture. It is a very specific type of headache known as a low-pressure headache, which worsens when standing and improves when lying down. It is caused by CSF leaking from the site where the needle was inserted.
Usually, a lumbar puncture headache resolves on its own within a day or two, but they can persist for longer. To reduce the risk of headache, you should try to lie flat for one to two hours after the procedure and drink plenty of water. Caffeinated drinks such as coca cola, coffee or tea may also help. If symptoms last more than a couple of days, a blood patch may be performed. This is where a small amount of your own blood is injected to seal the leak.
There is a lower risk of headaches and infections if the clinician uses a special atraumatic needle, such as a Sprotte or Whitacre needle. This type of needle has a blunt, solid, pencil-point tip, rather than a sharp cutting tip, which separates the tissue. Atraumatic needles are recommended by the British Medical Journal (BMJ) Rapid Recommendation panel, but are not always used. You can ask if you are concerned.
The immune system produces antibodies to fight infection. In MS, antibodies cross the blood-brain barrier and attack the myelin surrounding nerves. As a result, the level of antibodies in the cerebrospinal fluid of someone with MS is higher than it should be. Your CSF can be analysed to see if there are markers of inflammation present which are typical for MS. The following tests may be carried out.
If you have multiple sclerosis, then the number of white cells in your cerebrospinal fluid is usually up to seven times higher than normal. If the count is even higher than this, it is probably due to an infection of some sort, and not MS.
This is the test that has traditionally been used in the diagnosis of MS. The test uses a method called isoelectric focusing to look for oligoclonal bands (OCBs). OCBs are distinct patterns of antibodies – proteins made by the B cells of the immune system. A sample of CSF is placed on a gel and a voltage is applied. This causes antibodies of the same size to bunch together, forming visible 'bands'. One band (monoclonal) in the cerebrospinal fluid is normal. The term 'oligoclonal bands' refers to the presence of two or more bands and indicates disease activity.
If your CSF sample is going to be tested for OCBs, a sample of blood will usually be taken at the same time as you have your lumbar puncture. The cells and clotting factors are removed from your blood, leaving the serum which will be tested at the same time as your CSF for comparison. If OCBs are found in the CSF, they indicate inflammation in the central nervous system. If OCBs are found in your CSF but not in your serum, or if there are more OCBs in your CSF than your serum, this can indicate MS.
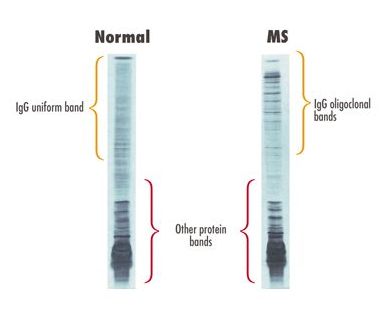
Over 9 in 10 people with MS have OCBs in their cerebrospinal fluid. But OCBs are not specific for MS and have been described in other conditions including viral encephalitis, bacterial meningitis and lupus.
This test alone cannot confirm or rule out MS, as up to 1 in 10 people diagnosed with MS will have a normal result with no OCBs present.
More recently, kappa free light chains (kFLCs) have emerged as biomarker for diagnosing MS. They are small protein fragments made by the antibody-producing B cells known as plasma cells. Normally they are assembled into antibodies, but if there is inflammation in the central nervous system, an excess of light chains is produced which are released into the CSF. Your CSF sample may be tested to see if you have elevated levels of kFLCs which could indicate MS. Unlike the OCB test, the kFLC test does not require a blood sample to be taken and tested for comparison.
We expect that in the future this test will be used more routinely than the one for OCBs as it is quicker and easier to perform.