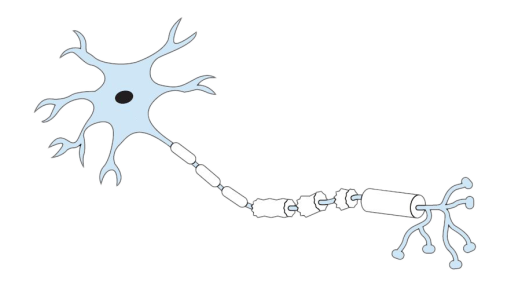
Multiple sclerosis is thought to be an autoimmune condition resulting in nerve damage through demyelination. Myelin is the substance that coats nerves, and demyelination means removal of this covering. However, MS is not the only condition like this, and it can be hard to distinguish MS from other autoimmune demyelinating syndromes (ADS), which are sometimes thought of as 'MS mimics'. Your neurologist may be considering these other conditions that might also fit your symptoms and medical history while you go through the diagnosis process.
To complicate the picture further, you may have had a diagnosis of one demyelinating condition before later getting an MS diagnosis. Conditions like optic neuritis (ON) and transverse myelitis (TM) can be conditions on their own, which may or may not eventually progress to MS. Getting the diagnosis right matters because giving the wrong treatment can make some demyelinating conditions worse.
A recent study followed 667 people investigated in Italian hospitals for symptoms suggestive of MS. Three years after their initial referral, 401 had a diagnosis of MS, 40 had neurological damage thought to derive from vascular problems (e.g stroke), 24 had a diagnosis of migraine with atypical lesions, 14 had a diagnosis of NMO (neuromyelitis optica) and 6 had been diagnosed with ADEM (acute disseminated encephalomyelitis) . It's also worth noting that 101 further people in this study had a diagnosis of CIS after 3 years, and a further 28 were still under investigation. This gives you an idea of the relative frequency of some other conditions that might mimic MS, and how long it might take doctors to reach a clinical decision about your personal situation.
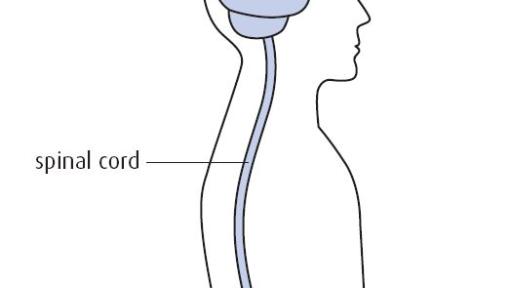
Transverse myelitis (TM) is a rare condition, affecting around 300 new people each year in the UK. It involves inflammation in the spinal cord which can damage your myelin and leave permanent scars or lesions. ‘Transverse’ refers to the inflammation being across the width of the spinal cord, although it often does not affect the whole width. 'Myelitis' means spinal cord inflammation. The lesions caused by TM can affect communication between the nerves in the spine and the rest of the body.
Most people with transverse myelitis experience muscle weakness, back pain, unusual sensations and numbness. At its most severe, TM can cause paralysis. The location of the lesion in the spine determines where in the body the symptoms will be felt. Bladder, bowel and sexual problems are common as nerve messages have furthest to travel to reach these areas, and are very likely to be interrupted, wherever the lesion is.
TM can happen to anyone, from infancy to later life, and men and women are equally affected. TM can come on over several hours, resulting in severe symptoms within 48 hours. However, some people develop symptoms more slowly over weeks or months.
In most cases, a person only has a single episode of symptoms. However, TM can be the first presentation of MS or another condition. You may be asked to undergo tests to establish whether you have antibodies in your CSF (spinal fluid) that might indicate that you are likely to have further episodes, in which case MS might be a more suitable diagnosis. Part of the diagnosis of MS is that it affects different areas of the central nervous system at different times. Between 13% and 63% of people with TM ultimately receive a multiple sclerosis diagnosis as well, and these tend to be those people who first noticed symptoms at a younger age.
Neuromyelitis optica spectrum disorder (NMO or NMOSD)
Neuromyelitis optica (NMO) or Neuromyelitis optica spectrum disorder (NMOSD) are also sometimes known as Devic's syndrome. The names all refer to autoimmune demyelinating conditions that affect predominantly the optic nerve and the spinal cord. As a result, the symptoms you get with NMOSD are generally optic neuritis (ON) which can affect one or both eyes, and transverse myelitis (TM), but with a relapsing remitting pattern. As with multiple sclerosis, NMOSD affects more women than men.
NMOSD is often associated with a specific antibody (AQP4-IgG or Aquaporin 4 Immunoglobin) that can be found in spinal fluid (CSF). This is another reason why a lumbar puncture can be part of the investigation for all demyelinating disorders, including MS. Finding this antibody would lead the neurologist towards an NMO diagnosis rather than MS, and they can then provide the right treatment.
People with NMOSD are usually advised to treat acute attacks with high dose steroids (intravenous methylprednisolone) and take an immunosuppressive medication for several years afterwards. This might be rituximab, azathioprine or mycophenolate. Some MS DMDs, including the beta interferons, Gilenya (fingolimod) and Tysabri (natalizumab), if given to a person with NMOSD, can make their condition worsen.
Acute dissemimated encephalomyelitis (ADEM)
Acute disseminated encephalomyelitis (ADEM) is a type of encephalitis, or brain inflammation. ADEM is more common in children than adults, and the peak age of onset is between 3 and 10 years old, although it can occur at any age. It is fairly rare, and an average local hospital would normally see only 1 or 2 cases each year.
Usually, ADEM follows an infection of some sort about 2-4 weeks beforehand. Such infections may be ordinary and mild such as a cold, sore throat or tummy upset. The immune system overreacts to this infection trigger and causes inflammation of the nerve coverings (myelin).
ADEM usually starts suddenly with symptoms that can be severe and worsen quickly. Headache, vomiting, drowsiness and neck stiffness are all common. A person with ADEM might experience loss of balance and inability to walk or stand. Seizures (convulsions or fits) can occur in up to one third of children, but they are not usually difficult to control. A child with ADEM is likely to be moved to a specialist children's hospital for care and rehabilitation.
Normally, ADEM only happens once, and when it is over it is over. However, a small proportion of children with an ADEM diagnosis may go on to develop MS, and research is underway to try to establish a better understanding of this risk.
-
Papetti L, et al.
Predictors of Evolution Into Multiple Sclerosis After a First Acute Demyelinating Syndrome in Children and Adolescents.
Front Neurol. 2019 Jan 15;9:1156
Full article (link is external)
Presas-Rodriguez S, et al.
Myelitis: Differences between multiple sclerosis and other aetiologies.
Neurologia. 2016 Mar;31(2):71-5.
Summary (link is external)
Karussis, D
The diagnosis of multiple sclerosis and the various related demyelinating syndromes: a critical review.
J Autoimmun. 2014 Feb-Mar;48-49:134-42.
Summary (link is external)
Cobo Calvo, A et al.
Idiopathic acute transverse myelitis: outcome and conversion to multiple sclerosis in a large series
BMC Neurol. 2013; 13: 135.
Full article (link is external)
Crout TM, Parks LP, Majithia V
Neuromyelitis Optica (Devic's Syndrome): an Appraisal.
Curr Rheumatol Rep. 2016 Aug;18(8):54
Summary (link is external)
Calabrese M et al.
"Better explanations" in multiple sclerosis diagnostic workup: A 3-year longitudinal study.
Neurology. 2019 May 1.
Full article (link is external)